New Cases.
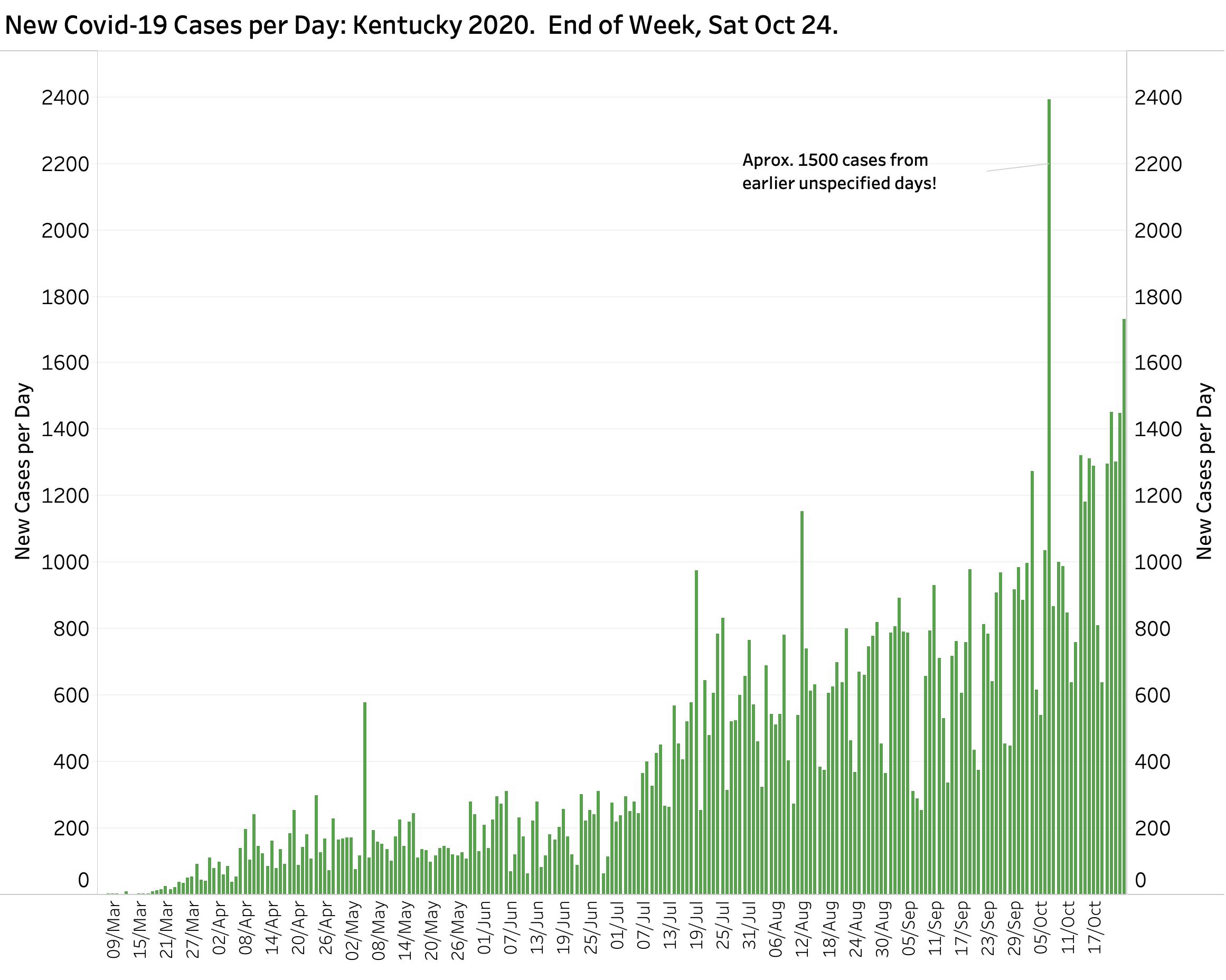
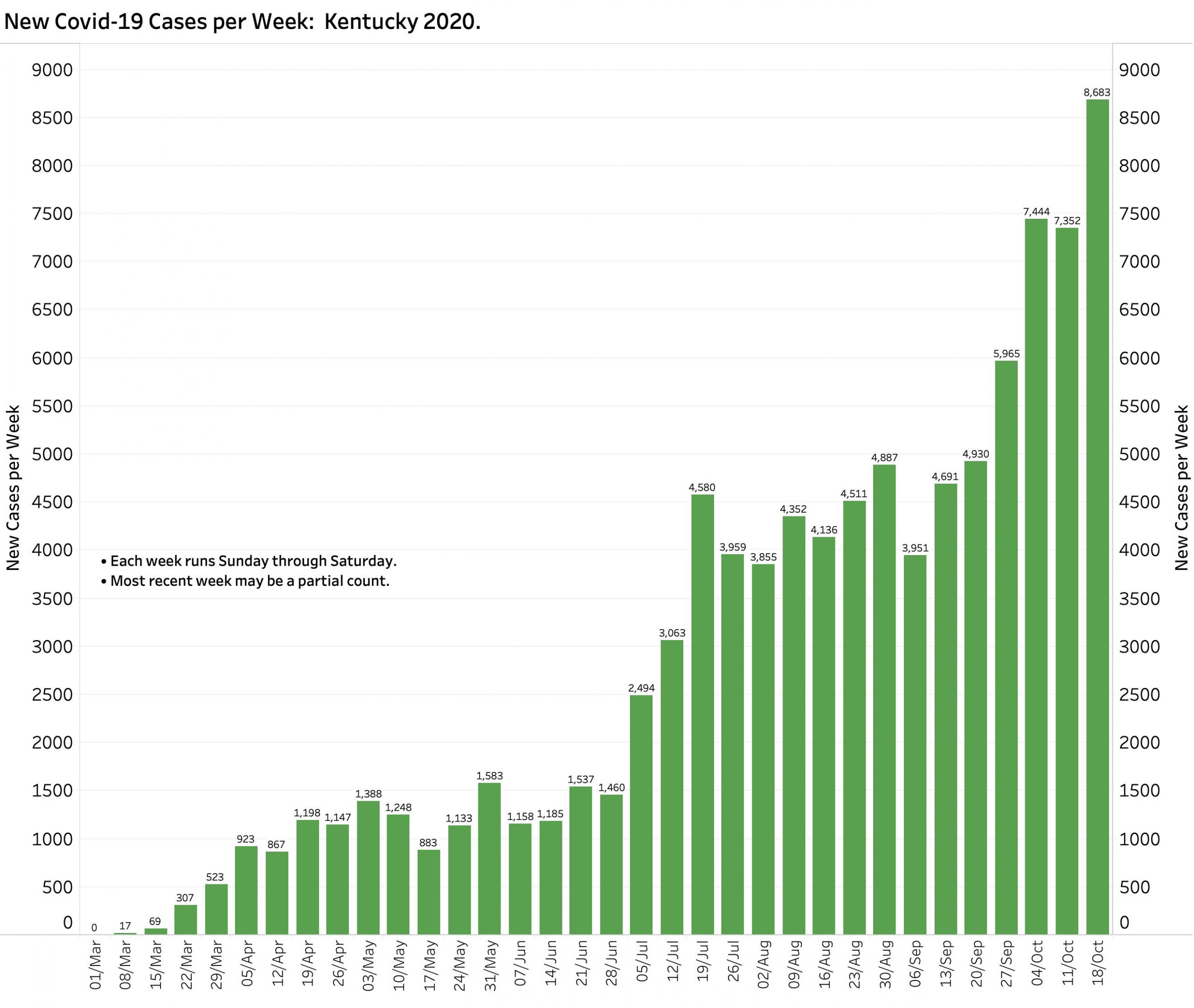
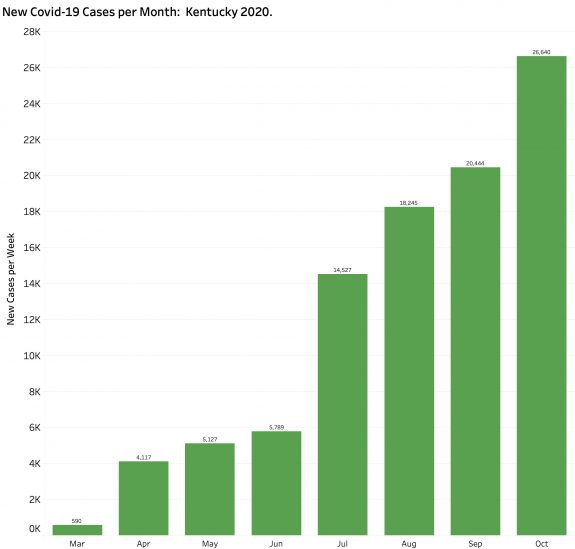
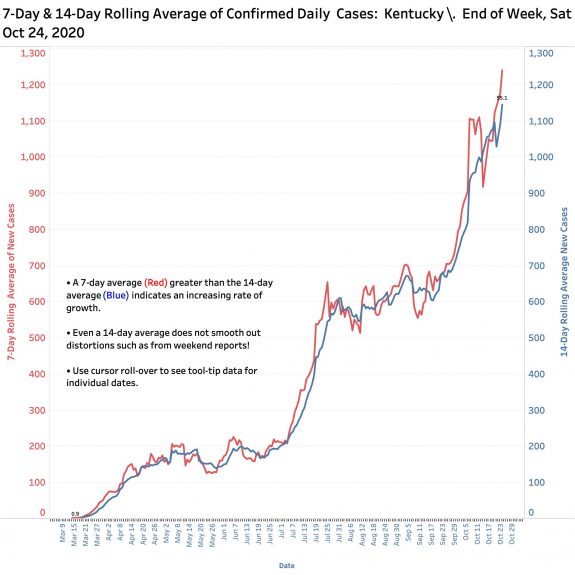
There is nothing good to be found in this End-of-Week report bracketed by Saturday’s released numbers. The 1732 unique new cases announced yesterday are by far the highest for a single day (save for the catch-up reporting of 1500 cases earlier in the month not assigned to a specific previous day). The 8683 unique new cases of the week leapfrogged over the previous weekly high by 1239 cases– a 17% increase. With 26,640 new October cases as of Saturday the 24th (and the month not even done yet) we already have 30% more cases than in all of September. Both the 7-Day and 14-Day rolling averages of new cases are also at record highs for the year. Since Sept 1, the aggregate total of new cases has been doubling every 5-6 weeks, a rate that is now worsening.
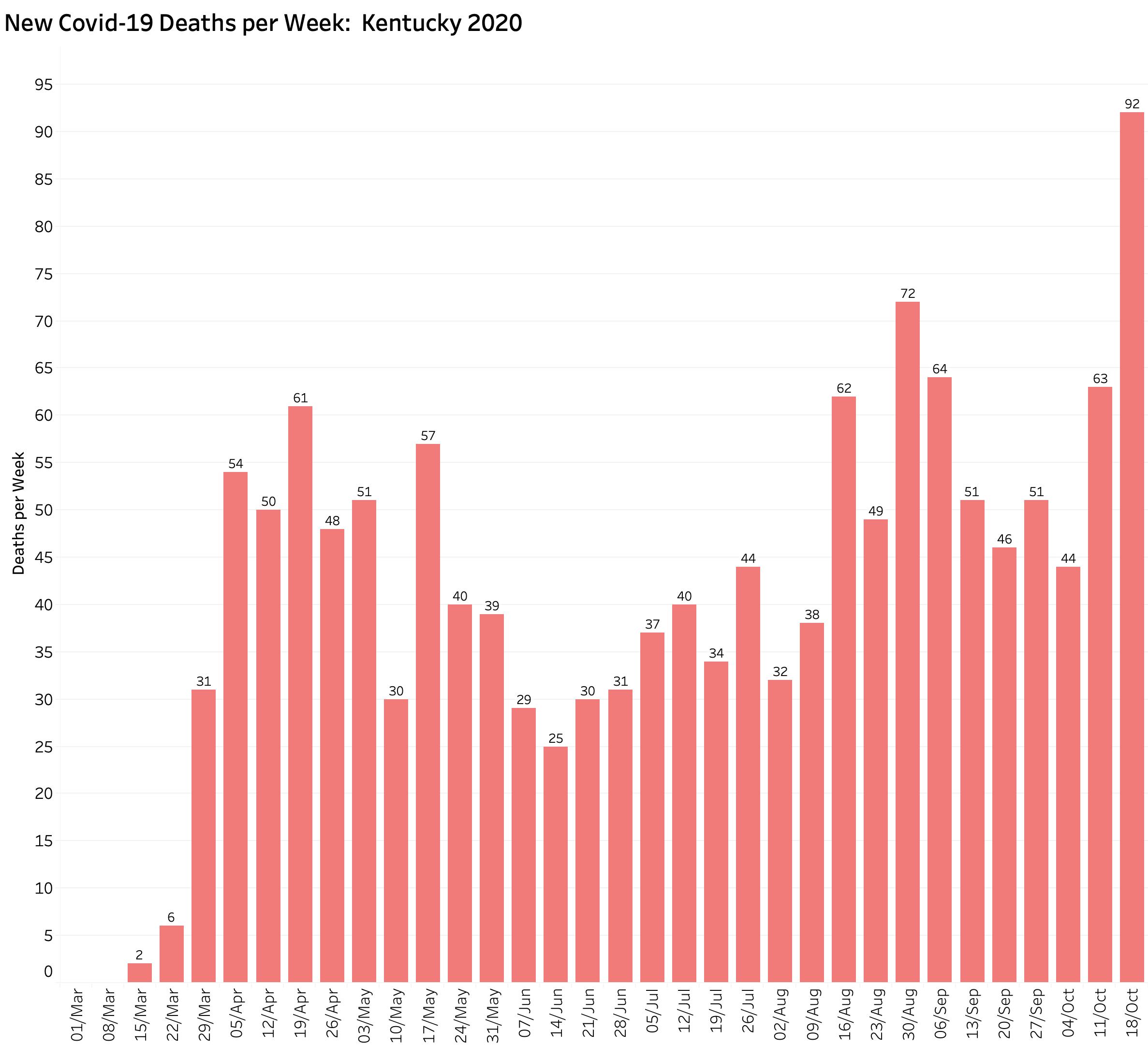
Deaths.
The 92 new deaths last week also set to a new weekly high for the year. It was 28% higher than the previous record of 72 deaths set during the week beginning August 30. As of October 24, we were only 11 deaths short of setting a new monthly record. There is little doubt we will do so.
Covid-19 Testing.
The Testing Positivity Rate (TPR) rose above 5.0 last week. However, since October 19 that figure began to be calculated using different definitions of case and test such that the significance of that increase remains to be seen. In any event, the TPR says more about the adequacy of testing rates than it does about the prevalence of disease in the population. It is with new cases, deaths, and hospital utilization that the rubber meets the road. In this last metric that we also set new records last week.
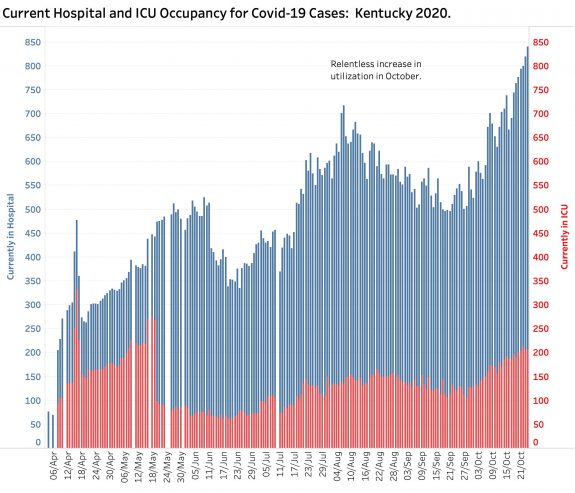
Hospital and ICU Utilization.
With 840 Covid-19 cases hospitalized as of the end of last week and 208 in ICUs, we have also hit new records. Given that there were obvious reporting problems from hospitals in the early days of our Kentucky epidemic, our current measures of hospital utilization also set new records for the year. As with Covid-19 deaths, hospitalizations begin to rise with a delay after new cases appear. Given the fact that increasing clinical experience with the disease has improved treatment and may be keeping patients out of the hospital overall, the current trend in increased hospitalizations is ominous. There are only so many beds in the state and they are now not where we need them. (More on this later.)
We are not alone.
Nationally and internationally, the Coronavirus that causes the disease Covid-19 is rebounding in many countries and now is worse than ever in the United States. Other countries that were reasonably successful in “flattening the curve” are essentially having to start over– or at least to be more aggressive with targeted interventions for local outbreaks. In Kentucky, we never knocked the disease down to a “flat” status. We left our springtime “plateau” with a second “surge” in early July that essentially tripled our daily new-case rate. Our new case rate sort of stabilized at this higher level through August and mid-September when it doubled with vigor and no signs that we are slowing down. In fact, as the colder weather drives our interpersonal activities indoors, and as we enter the season of respiratory disease, it is generally thought that darker days are ahead of us both literally and figuratively. I will not dwell here and now on the reasons we are in this sorry place. I believe, as do many experts, that it did not have to be so bad. Suffice it to say that both recognizing and owning how we got here is essential to finding our way out.
A different epidemic now.
Over the first 8 months of the pandemic in the United States, the most dramatic change in the dynamic of its spread is that Covid-19 is now expanding faster in rural and sparsely populated areas that had been relatively spared previously. At the start, as gateways to the larger world, it was in urban areas where increased interactions between people allowed the disease to gain an toehold. Today, virtually every county in the nation has been seeded with enough cases to maintain and indeed to increase the momentum of epidemic expansion. I and others have documented this for Kentucky. It was only a predictable matter of time. States with the highest per capita number of new cases now include North and South Dakota, Montana, and Idaho. Reports from these states and others (including Kentucky) speak of hospital and other facilities becoming overwhelmed with Covid cases. The Wall Street Journal, New York Times, other major national journalism outlets, and Covid-19 data-aggregating entities are telling the same story. It is being reported today that hospitalizations are up 40% overall, but compared to when was not clear to me.
Recall that concerns about taking care of current cases has been a major factor world-wide and here in determining the necessary level of effective public health interventions. When hospitals and their staffs get overwhelmed it is clear that bad things happen to both Covid-19, other patients, and their families alike! What happened in Northern Italy and New York City are verifiable examples of how social and professional standards and social expectations were challenged (i.e. who should be on a ventilator or transferred out of the ICU? Can I say goodbye to Grandpa?) The surge of cases in rural locations raises the critical issue of whether a mismatch is arising between where new Covid-19 cases are coming from, and the availability of acute care facilities and specialists needed to deal with the wide range of problems that Covid-19 brings.
How are our Kentucky hospitals doing?
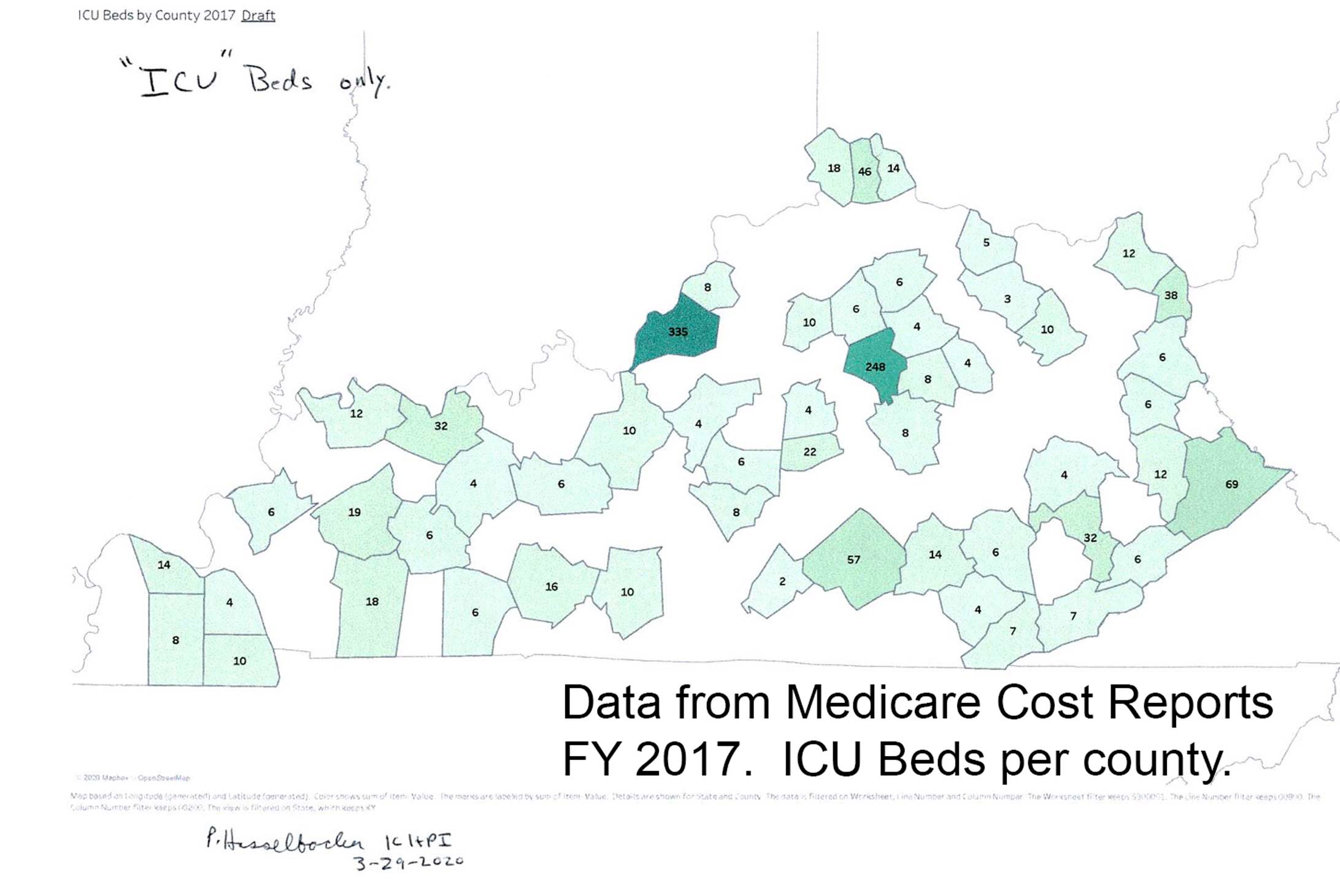
I do not know. I cannot tell. Raw statewide counts are insufficient to inform. It is the capacity of a given hospital that is the critical determinant. Early in the epidemic I was asked by a local journalist how many ventilators the state had available. I tried hard but could not find an answer. Indeed, I found it difficult enough to reliably determine the number of Intensive Care Units and ICU beds in the state. Reports from Frankfort related to hospital certificate-of-need provided this information for every acute care hospital, but these reports (like most other public-use files) are usually outdated to some degree. Specific information was available in the Medicare Cost Reports that all participating hospitals must file, but these were already two years out of date and presented me the most difficult data extraction challenges I have ever encountered. (I post one effort at the end of this article.) The CDC once posted a dashboard of hospital and ICU utilization which contained maps and counted beds, but inexplicably stopped doing so in July.
Counting is not enough.
My short preliminary answer to the question of how many ICU beds we had in Kentucky before the pandemic is that we may have had at least as many per capita as most other states, but they are not evenly distributed geographically or necessarily located where they are needed. I just pulled up the 2019 Kentucky Annual Hospital Utilization and Services Report for the calendar year 2019– the most recent tally available to me. It breaks down how hospital beds are distributed by type of bed for individual hospitals by Area Development District (ADD) but not county. Fully 50% of all Medical/Surgical ICUs in the state are in the Louisville or Lexington ADDs of KIPDA and Bluegrass. This is not surprising as this is where many of our people are. Eight of the 16 ADDs have 50 or fewer of these general ICU beds of which not all may be suitable for the care of, or have the staff needed by Covid-19 patients. The three counties of Northern Kentucky where there have been large numbers of cases have only 66 beds among them. Warren County, one of the counties with the highest numbers of cases in the state, has only 34 Med/Surg ICU beds. (There are only 50 ICU beds listed for the Barren River ADD of which Warren County is part.) King’s Daughters Medical Center in FIVCO has 32 of these ICU beds and may have been the first Kentucky hospital to declare that it was being overwhelmed. I will breakdown the paper documents from this report by county and hospital to make it easier to visualize a comparison of cases with beds.
Recall that there are quite a few Kentucky hospitals that do not have ICUs at all and that not everyone who needs an ICU bed has Covid-19. The small Medicare Critical Access hospitals which are limited to 25 total hospital beds and which serve the acute medical needs of many Kentuckians have no ICUs. In 2013 there were 29 of these, making up almost one-third of Kentucky’s hospitals. (I do not think they have all survived to 2010 or will continue to do so.) Hospitals have some ability to repurpose beds for emergency or other justifications. I spoke with one of the directors of a rural Kentucky Public Health Department about how I should interpret the raw reports of bed counts. What I was told was that when it was needed to know, a phone call to the hospital was required. However, it occurs to me that it may not always be in the best existential financial interest for a given hospital to admit that it is “overwhelmed” or at maximal capacity. After all, there are non-Covid patients that are seeking places to go for care who may revise their decision of where to go– or not go at all– for help.
I propose that the Commonwealth make available hospital capacity information to guide all decision makers and to justify sound recommendations for indicated public health interventions generally, or for a given area. For recruitment of public support for our ongoing effort to beat back our epidemic, the public deserves to know something more from case tracking efforts such as where new cases are coming from and who or what group is infecting who in general terms. If we are being asked to do hard things, I suggest that we deserve to know who and to be given the assistance to comply. Nationally we are not seeing that and locally I think we could do better. Raw case and death counts have not be enough to convert the sceptic, but now that the virus is in everybody’s back yard, even the reluctant should be primed to listen.
In the meantime, below is a map I prepared from Medicare Cost reports last March. You can review the full panel of graphics, updated regularly on the KHPI Tableau Public website.
Peter Hasselbacher, MD
President, KHPI
Emeritus Professor of Medicine, UofL
October 25, 2020

[Addendum Tuesday Morning, Oct 27, 2020]
Sunday and Monday numbers have been reported. The bad news continues in Kentucky, the United States, and many countries in Europe and elsewhere where record counts of cases appear daily. It is almost like we are starting over! More Rural US states reporting hospital capacity issues including Utah.
Kentucky’s 7-Day rolling average of new cases yesterday [following increasingly high case reports on Sunday and Monday] hit a new record of 1394 cases per day. It will take only 6 more deaths before the end of October to set a new monthly record for that outcome– and this before future deaths catch up with the prfesent cases. Hospitals are getting hit harder than at any time in the Kentucky epidemic.
PH