It is easier to give than to receive in the transplant world.
 In a comment added to a recent article about the current financial status of Catholic Health Initiatives (the parent company of KentuckyOne Health) it was alleged that Jewish Hospital in Louisville did not accept Medicaid patients for organ transplantation. Because of the seriousness of this allegation, I was reluctant to allow it to stand without further comment. I therefore did some research and elicited comments from involved parties. The results trouble me and highlight yet another major example of the disparity of access to health care in our inherently unfair non-system, dividing Americans as it does by socio-economic status. In the case of transplantation, the operational result is particularly ugly, because the weight of government regulation and community has given us a morally indefensible result analogous to the rich stealing organs from the poor. I call this an example of the “Reverse Robin Hood” nature of America’s National Health System! Neither Jewish Hospital nor UofL are responsible for this situation, but have benefited from it.
In a comment added to a recent article about the current financial status of Catholic Health Initiatives (the parent company of KentuckyOne Health) it was alleged that Jewish Hospital in Louisville did not accept Medicaid patients for organ transplantation. Because of the seriousness of this allegation, I was reluctant to allow it to stand without further comment. I therefore did some research and elicited comments from involved parties. The results trouble me and highlight yet another major example of the disparity of access to health care in our inherently unfair non-system, dividing Americans as it does by socio-economic status. In the case of transplantation, the operational result is particularly ugly, because the weight of government regulation and community has given us a morally indefensible result analogous to the rich stealing organs from the poor. I call this an example of the “Reverse Robin Hood” nature of America’s National Health System! Neither Jewish Hospital nor UofL are responsible for this situation, but have benefited from it.
The solid organ transplantation program at Jewish Hospital is one of only two such centers in Kentucky. (The other is 78 miles away in Lexington at the University of Kentucky.) Although it has been staffed professionally with faculty from the University of Louisville, since its inception, the Center’s administration and marketing have been firmly in the hands of Jewish which promotes it as an example of the high-tech status of its hospital. Organ transplantation programs pay well and enhance reputation. We have already seen how having transplantation programs gives a boost to hospitals in some quality ratings.
Transplantation of solid organs such as kidneys, hearts, lungs, and livers has moved beyond the experimental stage to become the standard of medical care for many conditions. It is common knowledge however, that there is a shortage of donated organs compared to the justifiable demand. We are all exposed regularly to entreaties to donate. Our state and local governments facilitate this process in several ways such as linking the process of obtaining prior consent to donate with applying for a drivers license. The Federal Government designates Organ Procurement Organizations around the country to coordinate the process of obtaining organs and distributing them to transplantation centers. Furthermore, hospitals that participate with Medicare and Medicaid are required by federal regulation to ask the families of potential donors for consent to remove organs when brain or cardiac death is present or anticipated. Everyone is potentially in the pool of eligible donors— rich and poor alike. I have written about this dichotomy before, but I have seen no additional public discussion.
Complicated organ distribution system.
For donors, eventually a point is reached when the interests of the organs take priority over interests of their current owners and then it is the organs that receive advanced life support. Once death has occurred or been pronounced, the organ is offered to the next eligible transplantation center identified through an algorithm that combines multiple medical and non-medical factors too complex to fully describe here. The fairness of the organ allocation process has been prominently and self-servingly disputed by hospital lobbyists. Given the scarcity of organs, I doubt that a solution acceptable to all centers exists. Money and status compete with the desire to do good.
Objective disqualification.
Transplantation centers evaluate patients who have applied to be on their waiting lists both before acceptance and after a potential organ becomes available. Some of the factors considered in this rationing process are fairly objective and defensible from a medical science perspective. For example, the blood type and transplantation antigens of donor and recipient must be compatible. Particularly in the case of children, the organ may need to be of a particular size. There are few issues of ethical concern here.
Financial Status a Barrier to Organ Transplantation But Not Donation.
Some factors considered involve value judgements but are considered “medically” justifiable. For example, liver transplants are regularly denied to patients who continue to abuse alcohol, and lung transplants to those who still smoke tobacco. Infection with HIV or hepatitis virus has been used in the past to strike the eligibility of potential recipients on the the grounds that their infections cannot be cured and that the transplanted organs will be reinfected. Such factors are written into benefit coverage restrictions by insurance companies. While such rejections of eligibility may be couched as rational, they nevertheless balance the value of the organ against the life of a potential recipient. That is what rationing is supposed to do. I am using the word “rationing” provocatively, because isn’t that what we are really doing with this scarce resource? That doesn’t make it wrong, it only magnifies the need to make the process fair!
Subjective disqualification.
Some of the factors considered for acceptance to waiting lists are clearly more subjective such as the age, co-morbidities, overall physical status, cognitive ability, or mental health of the recipient. How old is too old? How sick is too sick? How mentally ill is too mentally ill? Will the recipient be able to comply physically or emotionally with the demands of post-transplant life? Will there be enough family or psychosocial support to ensure a successful result and sufficient improvement of quality of life?
Financial disqualification.
Ironically, the most objective of all criteria used to determine the eligibility of an individual for transplantation is the most discriminatory— the wallet biopsy. The evaluation of a potential transplant recipient includes their financial status and whether the patient has sufficient insurance coverage to pay their way. Simply having medical insurance is not enough. For example, it was standard practice in the past at Jewish Hospital and at least some other hospitals not to transplant Medicare patients who could not afford the anti-rejection and other medicines necessary to maximize the survival of the transplanted organ. Inability to afford such post-transplant expenses is still on the list of factors considered by some or even many transplant centers.
What does it cost?
The charges for organ transplant are among the highest for all hospital discharges. According to the respected healthcare firm Milliman as presented on a UNOS website, in 2011 the average aggregate billed charge for a transplant including pre-testing, procurement, surgery, and followup ranged from $26,200 for a kidney, to a $Million or more for heart or intestine. Of course, transplant programs are willing to accept less. When I was a former insurance executive in the mid-1990s, I was able to negotiate the charge for bone marrow transplant at a Cincinnati hospital down by 50% with a simple telephone call. The uninsured do not have an insurance company intermediary working on their behalf! They may be presented with the whole bill.
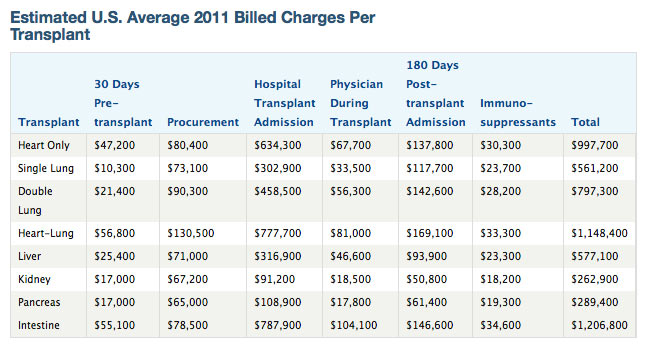
Of course, even for the insured, there are increasing deductible and copays that have to be paid. That’s why we still see so many coin canisters and bake sales in our communities supporting those hoping to receive a transplant. If you are independently wealthy, cost seems not to be a factor, giving rise to occasional public expressions of skepticism that some seem to be able to jump the transplant line while others die every day waiting for an organ. Of course, the cost of the actual transplantation is not the end of it. A transplant recipient becomes a professional patient and a financial annuity for the transplant program. Costs persist for the remainder of the patient’s life.
Medicaid: Is having insurance enough?
Obviously some transplant centers are willing to accept what private insurers have negotiated to pay. I contacted Kentucky’s Department for Medicaid Services in Frankfort. A spokesperson told me that “All medically necessary organ transplants are covered by Medicaid and our MCOs. There are no Medicaid restrictions, other than medical necessity. Medicaid pays a standard reimbursement of $75,000 for heart, bone marrow, liver and lung transplants, and may pay more for other transplants or under certain circumstances. …There are no out-of-state restrictions, other than the Provider having a KY Medicaid ID number.”
The difference between what Medicaid pays and private insurers pay is what hospitals commonly refer to as “under-reimbursed” services. It is possible, even probable that some transplant programs would not consider Medicaid’s reimbursement to be adequate. It is unclear to me at the moment if the private Medicaid Managed Care plans in Kentucky reimburse more or less for their members than the Commonwealth does for the beneficiaries still managed directly by the state.
Medicare.
I do not know what Medicare currently pays for organ transplantation. Even if the surgery is covered, my guess is that many Medicare drug plans and certainly many private insurance plans leave people pretty unprotected against the costs of anti-rejection drugs. As an exception, it is my understanding that federal law requires Medicare to cover costs of kidney transplants, and that includes virtually everyone with chronic kidney failure who automatically become eligible for Medicare’s chronic renal disease program. This is in itself a form of discrimination by organ against patients for whom transplantation is medically indicated! If government enforces the structure and rules for both organ donation and transplantation that effects all citizens, it needs to pay for it.
KentuckyOne Health.
I asked a spokesperson for KentuckyOne Health if “Medicaid patients enrolled in any of Medicaid managed care programs or those outside the Medicaid Managed care programs are being excluded from organ transplantation at Jewish Hospital?” In response I received the following:
“KentuckyOne Health accepts both Medicaid and Medicare for the organ transplant program at Jewish Hospital, although eligibility may be impacted by specifics of individual plans.”
I also questioned some of my UofL surgical colleagues who confirmed that financial considerations play a role in who receives an organ transplant in Louisville. It was suggested that a hospital cannot be expected to “donate their services.” In my opinion, these comments allow that at least some, if not many Medicaid patients are not accepted to the transplant waiting list at Jewish Hospital for financial reasons. My guess is that this circumstance would not be unique among transplant centers nationwide, but I do not have specific data in hand. I would appreciate more definitive information from my readers. I will also try to find actual utilization data.
University of Kentucky Transplant Program.
I made a similar request of the transplant program at the University of Kentucky. I was told that “as an agency of the Commonwealth, UK accepts Medicaid insurance as payment for transplantation.” (I was told essentially the same thing 15 years ago.) No equivocation was apparent, but I do not yet have confirmatory utilization data in hand to compare payer mix at the two Kentucky transplantation programs, or for that matter for the rest of the nation. [See a later article for this information.]
Aside.
I could not help but reflect on the current legal dispute between UofL and Norton Healthcare in which UofL seeks to evict Norton from Children’s Hospital. One of UofL’s chief arguments is that it is an agent of the state, yet it has given the bulk of its clinical services over to KentuckyOne Health that most assuredly is not. Ironically, UofL also seeks to block the University of Kentucky from providing clinical services in Louisville. The self-defeating result of giving its clinical services away to a private organization is that UofL is causing organ transplant patients to be referred to Lexington for their surgery! Indeed, I have been told privately by a knowledgeable colleague that they are no longer confident of KentuckyOne’s commitment to transplantation. What a change that would be!
How can this stand.
I hardly expect any medical program to come right out and say they turn the poor away from their doors, but of course that happens every day in virtually every city. My examination of the medical and lay literature, and my inquiries within our state have convinced me that being poor is a major non-medical impediment to receiving a life-saving organ transplant. For example, a study published in 2008 by Herring et. al., looked at a nationally representative sample of hospital discharges. They found that 16.9% of organ donors were uninsured, but that only 0.8% of transplant recipients had no health insurance. Their conclusion: “Many uninsured Americans donate organs, but they rarely receive them.”
Naturally, being poor (or for that matter being an uninsured middle-class Joe or Jane) does not diminish ones ability to serve as an organ donor for the benefit of someone else! Indeed a recipient’s health insurance will likely cover the expense of extracting a donor’s organs and keeping them alive until they are used. That the full weight of government and the turning of a blind eye by the public keeps this travesty of justice alive, is in my opinion, a disgrace. I would welcome a comment by anyone willing to put their name beneath a different opinion or justification.
We can do better. For example, the national health program of Spain covers transplantation for all its citizens. It also has laws that presume a general consent to donate organs. Medical necessity and appropriateness alone is said to determine who gets a transplant. Many fewer patients die waiting for organs. The World Health Organization rates the Spanish health system as superior to ours but costing less.
As I look through my morning newspapers, I am increasingly aware of how many of the difficulties we ascribe to our employer-based health system could be fixed or ameliorated by a single-payer national health system. Despite the mean-spirited accusations of some in congress, what else is health insurance supposed to do but spread the resources of the mostly well in support of the needs of the few. This is not, and never was a secret.
As for now, and for all of us who may someday require an organ transplant— “May the odds be always with you.”
Peter Hasselbacher, MD
President, KHPI
Emeritus Professor of Medicine, UofL
November 24, 2014 (Thanksgiving week!)
As always, if I am incorrect or unclear in any of my facts, please also let me know.

The need for insurance for transplantation is a problem in the United States and unfortunately will continue to be one.
A recent article sent surveys to heart transplant programs across the US regarding their requirements for insurance. Here is the manuscript’s title:
Thibodeau JT, Rao MP, Gupta C, et al. Health insurance as a requirement to undergo cardiac transplantation: a national survey of transplant program practices. Transplant Proc 2013;45:360-3.
84% of heart programs who responded say they require insurance before they can list a patient. 81% say they require money upfront if the patient has no insurance.
10% of programs require a Medicare SUPPLEMENT to list a patient for transplant.
The exact practice of Jewish Hospital is not known to me, but I have had patients tell me they were turned down for transplant evaluation at Jewish because they had no Medicare supplement. KentuckyOne obviously knows that which is why they hedged when you asked them directly about insurance requirements re: Medicare and Medicaid.
The bottom line if you are dying at a small hospital and don’t have insurance and your doctor tries to refer you to Jewish Hospital for organ transplantation, you won’t be accepted there. This is the case at many hospitals across the country as well.