I have been interested in attempts to measure the quality and safety of healthcare since my year of fellowship on the Senate Finance Committee which oversees the Medicare program. In the run-up to what would become Medicare’s Hospital Compare program, a long list of things that might be measured was proposed. Most were set aside because of concerns about utility, comparability, reliability, difficulty of collection, or ability to be gamed. The shorter list evolved into the current iteration of Medicare’s own Hospital Compare database that is incorporated into virtually every proprietary hospital rating system. The quality measurements are part of a new payment structure that hopes to pay for quality and value instead of volume alone.
This month, the rubber hit the road. For an eligible 3300 or so acute-care hospitals for which a score could be calculated, CMS released a composite score of the frequency of Hospital Acquired Conditions and infections (HAC). The 25% of hospitals with the worst HAC scores “are elligible” have their total Medicare patient payments reduced by 1% beginning October, 2014. For technical reasons only 724 hospitals (fewer than 25% of hospitals) actually received the penalty. Attached is a list of the elements that are included in these actionable HAC scores. Note that some of the elements previously included in Hospital Compare such as retained object in surgery have been left out, much to the distress of some proprietary organizations. Infections resulting from intravenous lines and urinary catheters alone contribute to the majority of the overall HAC score.
I think the idea is great, I think the execution is difficult. Having examined the quality and safety scores of Kentucky hospitals by different organizations over time, I am concerned that there is excessive lability of scores. Using essentially the same Medicare data with different twists, different proprietary agencies will give the same hospital different rankings (occasionally drastically so) at the same time. Conversely, the same organization might give the same hospital a different score over a relatively short period of time. I also have concerns about the reliability of self-reported data. Although I expected that objective measurements might differ from my own perceived evaluations of hospital quality, I was quite surprised at the magnitude. I was concerned about the financial implications to both hospital and rating organizations. Therefore, at every opportunity over the last year, I shared my belief with experts that available measures of quality and safety were not ready for prime time. I was told my concerns were reasonable.
As I have done before, I extracted all the Kentucky hospitals from the national list in an attempt to get a manageable handle on the data. Attached is a list of Kentucky hospitals subject to penalties as ranked by their composite HAC score. Note that only 65 of our 100+ hospitals were vulnerable to the penalty. Some classes of hospitals such as standalone cancer, children’s hospitals, psychiatric hospitals, and others are excluded nationally. Also excluded are Medicare Critical Access Hospitals. These are small and mostly rural hospitals which are quite limited by statute as to what services they can provide. They are paid their costs plus 1%, nominally so that do not lose money on Medicare patients. CAH hospitals are not required to submit the same quality measurements to Medicare as other hospitals. God alone knows what happens there. There are some 30 CAH hospitals in Kentucky.
Some 3300 hospitals received scores ranging from 1 to 10 with 1 being best. There has been some confusion in initial media reports about the cutoff HAC score identifying hospitals that will have their total Medicare payments reduced. Jordan Rau, Senior Correspondent for Kaiser Health News, has been reporting extensively on this program and was very helpful to me. It did not help that the key Medicare file listing the individual penalized hospitals was unfindable by me with out Rau’s help! Further making analysis more difficult, the definitive Medicare file available so far lists hospitals by provider number, not by name. The short answer is that hospitals with a total HAC score greater than 7.0 take the hit.
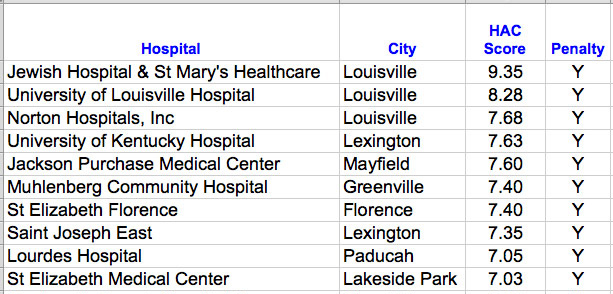
Only 10 of the 65 Kentucky hospitals were penalized. Compared to the rest of the country, Kentucky did better. Our average score was 4.9, better than 5.5 nationally. Surprisingly, disappointingly, and even sadly, many if not most of Kentucky’s most prominent hospitals will be penalized for alleged shortcomings in these measures of quality and safety! See complete list of Kentucky hospitals with their scores here. [Addendum and apology, Dec 23: For the initial posting of this article, I drew from a database provided by a prominent health-news organization that used an erroneous method of calculating the cutoff. Two additional Kentucky Hospitals with scores of 7.0 were listed as receiving the penalty– Rockcastle County and Three Rivers. I apologize for erroneously including them in the initial version of the table below.]
Louisville not a bright spot.
These are the Kentucky hospitals for which a 1% reduction in Medicare payments will be made at least until the next evaluation cycle.
In Louisville, our three major downtown hospitals/systems had the worst scores in Kentucky. (Medicare does not distinguish the Norton Healthcare, or Jewish Hospital & St. Mary’s Healthcare systems by their individual hospitals.) For perspective, a score of 9.35 or worse places a hospital among the poorest-rated 58 hospitals nationally, a score of 8.25 in the poorest 280, and a score of 7.675 with the poorest 474 hospitals. Even the Baptist Health hospitals that have done well in past rankings of quality escaped only by a whisker from being penalized. Both of Kentucky’s university teaching hospitals were penalized. However, even knowing these scores, I would personally have little trouble using some of the penalized Kentucky hospitals as either a doctor or a patient. Is something wrong here?
Is it fair?
Reasonable questions of fairness are being asked. It is difficult to argue that things like bedsores, infected intravenous catheters, urinary catheters, or surgical infections are immaterial. It is argued (especially by those with poor scores) that large urban or teaching hospitals that care for populations of disadvantaged patients are being disadvantaged themselves. Will taking money away help make things better? On the other hand, it is also reasonable to ask if a lower standard of care for poor people or teaching patients should be acceptable in our society.
Painful indeed.
As Hannibal Lector said before he chopped off his hand— “This is going to hurt!” Beginning with admissions in October 2014, 724 hospitals will have their total Medicare payments reduced by 1%. This may seem like a small amount, but most hospitals claim that even current payments do not cover the costs of caring for Medicare patients. According to the Medicare Payment Advisory Committee, the average hospital Medicare margin in 2012 for acute care hospitals was -5.4% for all hospitals, and -7.1% for nonprofits. If these numbers are justifiable, than all Medicare patients are financial losers for hospitals to begin with! Paradoxically, major teaching hospitals had margins of -2.6% compared to non-teaching hospitals at -7.2%. For-profit hospitals do “better” with a margin of +1.5%. Teaching hospitals are paid considerably more per patient than other hospitals because of bonuses for having residents, and for the higher rates of federal disproportionate care payments intended to offset losses for indigent care. [Not all disproportionate share payment rates are the same. Medicaid patients are worth more to some hospitals than others, a factor at the root of the claimed abuse of the 340B drug discount program, but that is a topic for another article!]
But my hospital’s patients are sicker and poorer!
Although it is asserted that the quality elements quantitated above have been adjusted for patient sickness, I also have my doubts about whether attempts to correct for severity of illness or nonmedical/socioeconomic determinants of health are ready for general prime-time clinical application. (Similar arguments are offered about the wisdom of the new policy of penalizing hospitals with high readmission rates.) I had the opportunity to examine the database of one of the flagship quality and safety rating organizations on the condition that I not publish any of the data. I concluded that while many large urban or teaching hospitals were able to score well, I could not rule out that some were handicapped by things they could not control. In my opinion careful attention needs to be given to what we might be doing to institutions that are seeing patients that few other hospitals are eager or even willing to accept.
You can already hear the howling in the streets.
So what will hospitals do now? No doubt they will try to do better. It is clear that when efforts are made to focus on proper care of intravenous lines or urinary catheters, that infection rates can be brought very low, but they will never be eliminated altogether. Hospitals should be trying anyway. It is troubling to contemplate that embarrassment or a financial club would be considered necessary to motivate hospitals and their staffs to do what is right or best. I do not think that is universally true. Most hospitals and their professional staffs want to do the right things. It cannot be denied however that some hospitals make it into the news for less noble aspirations. What will be depressing for hospital financial officers is the recognition that no matter how hard they try or how well they succeed, 25% of them will be penalized every year by the withholding of Medicare payments, the cost of which will inevitably be passed on to all of the hospital’s patients. Even more quality and outcome elements are scheduled to be added to the mix in the near future. Do we call this continuous quality improvement, or a regulatory treadmill? Will private payers follow Medicare’s payment lead or use the HAC scores to assemble narrower networks?
The take-away.
Does this mean that Kentuckians should not go to any of the penalized hospitals for healthcare services? Of course not. In any case, in the age of narrow networks and high cost, most of us have little geographic or financial choice in the matter. However, some of these hospitals have a lot of explaining to do. CMS itself needs to make a stronger case that all the regulation and paperwork makes a difference. If the scores are valid, then we have a clinical problem in Louisville and elsewhere. If the scoring system is flawed, then it needs to be scrapped. In my opinion, we are somewhere in between. All the above said, I still think that more transparency about clinical outcomes is justifiable and important. Indeed it is central to our efforts to evolve a better healthcare system.
As always, if I have made an error of fact or you have a better interpretation, let me know.
Peter Hasselbacher, MD
President, KHPI
Emeritus Professor of Medicine, UofL
December 20, 2014
Useful Links:
(Still being added)

As I began to dig into the nuts and blots behind the HAC scores it became evident that there has been some confusion about the cut-off score used to determine which hospitals were actually assigned the 1% cut in Medicare payments. My first iteration of this article erroneously used a score of 7.0 or higher. For technical and statistical reasons, the correct cutoff is scores greater than 7.0, but not including 7.0 itself. One consequence of this calculation is that fewer than 25% of eligible hospitals are actually penalized. More about this and a breakdown of the three components making up the aggregate score will be discussed in a later article.
I made the appropriate correction in the table of the article above.
[Addendum] After I wrote this I unpacked the entire HAC database from CMS that includes the individual composite scores that make up the two domains summarized in one of the attachments above. The non-uniformity of data collection stuns me! All hospitals in the list had a Domain 1 score. However, 1020 hospitals did not report incidence of systemic infection from intra-venous lines and 669 did not report urinary tract infections from indwelling urinary catheters. 662 Hospitals had no Domain 2 score at all! Is this a fair comparison? Scientifically, I would say that apples and oranges are being compared.
If this clinical study were being submitted to a medical journal, it would in my opinion be rejected. And yet it being used to effect the destiny of hospitals and the patients they serve! “Not ready for prime time” may be an understatement.
I will update the table of Kentucky Hospitals later and demonstrate by example how the non-uniformity of data collection influences the overall score.