Informed consent forms reflect Ethical and Religious Directives of the Catholic Church.
A recent report by Kate Howard of the Kentucky Center for Investigative Reporting on the withdrawal of federal funding for a University of Louisville research study conducted at Frazier Rehabilitation Hospital shines a bright light on how research –specifically research involving human subjects – is performed at the University of Louisville and in its partner institutions. The specific research protocol in question, directed by UofL faculty member, Dr. Susan Harkema, was intended to examine if adding the muscle relaxer Baclofen to a regimen of physical therapy on a treadmill improves or worsens function in patients who are partially paralyzed as a result of spinal cord injury. The study holds out what is in my opinion an insufficiently proven hope of a possible increase in ability to stand or ambulate. Many aspects of the study were criticized by both federal authorities and by the university’s own investigation. I believe those criticisms to be valid but will not address them in this article. In my own professional opinion, the study as designed and conducted had very little chance of producing meaningful data in any event.
Informed consent – The ethical core of human subject research.
Human subject research must be reviewed and approved by the University of Louisville’s research Institutional Review Board (IRB) using a rigorous national set of requirements and guidelines designed to put the interests of the research subject first. These rules comprise a ‘Federal Policy for the Protection of Human Subjects’ and collectively are called the ‘Common Rule‘. Violation of the Common Rule can result not only in grant support being withdrawn as it was here in Louisville, but in prohibition of future human subject research. To put things in perspective, this would be the equivalent of a death-sentence penalty from the NCAA. By contract, KentuckyOne has agreed to use the UofL IRB to supervise research performed in its facilities, including in University of Louisville Hospital.
Problems with informed consent.
The IRB’s own recent internal investigation revealed that that some Baclofen study participants signed the wrong consent forms. Specifically, this had to do with whether or not the research subject was aware that they would be personally responsible to pay for the (expensive) experimental physical therapy that is at the center of the research protocol. Initially some subjects were surprised to get very large bills for their participation on top of the unreimbursed travel and housing expenses required for the several-month study. The consent form had been changed by the IRB to make it clear that there were financial implications to participation.
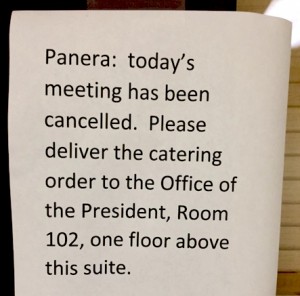
I too was concerned about the informed consent forms used, but for a very different and profoundly more significant reason. In my opinion, full informed consent was not being given. Additionally, the template consent form required by the University of Louisville’s IRB had been altered to conform to the religious tenants of the Roman Catholic Church – changes which I and others had been promised would not occur. If these alterations to the standard informed consent form template were made without the documented express permission of the IRB, this would constitute a major violation of research protocol and ethics. If my University’s IRB did in fact approve the changes, my earlier concerns have been realized and I am ashamed for it. Let me explain. Continue reading “Termination of Baclofen Study at UofL Discloses Influence of Catholic Health Initiatives on University Research.”