Who is getting paid for what? Why should we care?
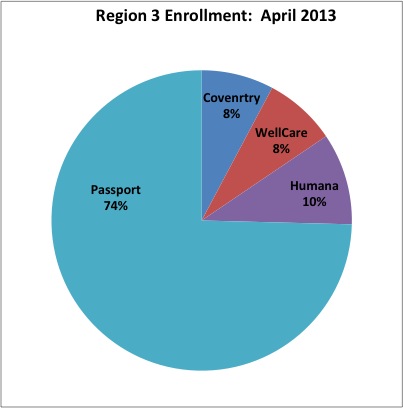
Some months ago I reported on the shifting enrollments of Medicaid Managed Care beneficiaries among the four Managed Care Organizations (MCOs) in Region 3, which includes Louisville and a few surrounding counties. Although the initial assignments by the state gave roughly equal numbers of beneficiaries to each of the MCOs selected to do business in the Region, Passport was able to leverage its previous home-court, sole-source advantage; and cooperation from its existing participating providers to recapture the lion’s share of patients from its new competitors. In this installment, I show the final enrollment figures as of April 2013 when the relatively unfettered ability of a member to change from one plan to another expired. The big winner continues to be Passport which expanded its Region 3 market share to 75% compared to 64% early last February.
Medicaid Managed Care was reintroduced elsewhere in the state in January 2012. In little more than a year, the distribution of enrollees outside Region 3 shifted to favor two of the three MCOs. (It didn’t help that one of the MCOs has already expressed interest in leaving the state.) Competition, as opposed to cooperation, produces winners and losers. The hope (and it remains a hope) is that patients will come out winners. I present some enrollment figures below as well as the rates paid by the state to the MCOs to cover the care of beneficiaries. A table of the data can be downloaded here.
Background: Different Programs for Different Folks.
In general, the federal Medicaid program tries to follow the principal of nondiscrimination. Although it is clear that the rules of coverage vary greatly among the different states that co-fund the program, in general, and within a state, everybody is supposed to be treated the same. Over the years, and in the search for ways to improve quality and to decrease cost of the state programs, the federal office has granted a variety of waivers or otherwise allowed experiments and variation to occur. Such special dispensations required beneficiaries and providers in Region 3 to participate in Medicaid managed care, even though the rest of the state could not get its act together to successfully assemble such a program–then or now! The University of Louisville’s new MCO, named Passport, was allowed to become a sole-source provider without competition. Although the University benefited greatly from its control of the finances of the program, Passport’s clinical operation also enjoyed real success, largely due to giving non-university providers some input in the clinical development and management of the plan. (Why should it be otherwise anywhere?)
The result has been that Passport was permitted to enjoy a monopoly for over 10 years despite considerable uncertainty over how much (if any) money was being saved by the state. In January 2012, with Medicaid costs to the state rising uncontrollably, a second initiative was launched to expand Medicaid managed care to the rest of the state. [It didn’t work the first time.] I and others have commented on the rocky road that has resulted. Following this statewide expansion and a scandal over the University of Louisville’s illegal use of Passport funds for its own purposes, Passport’s protected status was withdrawn and 3 other MCOs were allowed to serve in Region 3. The requirement that new MCOs serve the entire state was waived. At present, Passport and Humana operate only in Region 3. Kentucky Spirit operates everywhere except Region 3. Of course, the current status will change considerably as Medicaid eligibility expands under terms of the Accountablity and Affordable Care Act. For now, the playing field is quite uneven. History has proven how difficult it is to assemble a coordinated and efficient provider network out in the state. I cannot imagine the business lobby will permit competitive advantage to continue for much longer. [Click the Medicaid Tag below to see previous articles about Kentucky Medicaid.]
Additional thoughts:
Good news for Passport, at least for a while.
All the good news presently falls to Passport which increased its market share of Region 3 beneficiaries from two-thirds to three-quarters in less than two months. The period of facilitated voluntary transfer from one plan to another is over, but come open-enrollment season at the end of the year, who knows what will happen. Much depends on reputations that will grow or diminish before then, and what other MCOs enter or leave the local or statewide markets.
Region 3 still part of a state system.
Louisville is by far the largest city in Kentucky, and compared to the rest of the state, has hot and cold running doctors and other providers beating the bushes to find work. [What do you think all those billboards around town are for?] Nonetheless, the large majority of Medicaid beneficiaries in Kentucky’s managed care system reside elsewhere in the state. Region 3 has only 23.9% of Medicaid Managed Care beneficiaries– not even one quarter. Of course, not all Medicaid beneficiaries have been placed in managed care. I would appreciate some informed opinion about the numbers and financial impact of the excluded groups. For example, I understand that Medicaid beneficiaries in nursing homes are excluded from managed care but they are both numerous and expensive. Also, I do not know who gets paid when services not available in rural areas are provided in Region 3. Are extra transfer payments made? Do such payments come out of the money-pots of the transferring MCO? What happens when a Humana member requires admission to Kosair Children’s, a University-controlled institution? Does Humana get hit with the same non-discounted bill the uninsured individual gets? What would happen if Passport is required to or wishes to expand out into the rest of the state to capture increasing patient referral flows?
How many patients does it take to make up a lightbulb that glows?
For Coventry and WellCare that have an administrative apparatus already able (some claim) to manage Medicaid networks throughout the state, the additional fixed cost to provide services in Region 3 may be reasonable. (I do not mean to discount the difficulty in assembling provider contracts in hostile territory. After all, it was impossible to generate provider support elsewhere in the state 10 years ago, and some would argue even today.) For a Humana with only some 17,000 members in Region 3, the relative overhead must be colossal, even with an experienced Medicaid managed care partner doing the heavy lifting. I have to believe that Humana is disappointed in the current outcome– I would be. Humana has much experience in managing provider networks in Kentucky but may have had difficulty in convincing those providers to accept Medicaid patients. This has always been a problem in the free-market, fee-for-service structure. Part of it is that Medicaid, like Medicare, does not pay as well as private insurers or self-pay patients. In my personal experience it was always hard to find a specialist to take care of a Medicaid patient, let alone an uninsured one. The University of Louisville has traditionally filled that role in Region 3, albeit in facilities euphemistically called “teaching clinics.” Working with a group of committed providers experienced in caring for the socially-disadvantaged sick gave UofL and Passport a big leg up in their clinical success.
Healthcare reform will change everything– I hope!
Humana has solid resources and is no doubt in it for the long game. I suspect they and other national Medicaid MCOs are anticipating the wave of new Medicaid beneficiaries covered by Obamacare. These new potential MCO members will have less personal experience with the teaching-clinic and indigent care systems of Louisville and are likely to have expectations more in line with those of the privately insured. A Humana, or a Coventry, or a WellCare may be anticipating the opportunities of such a scenario here and across the nation– if they can only hold out financially in the meantime! Passport can benefit too, but in my opinion that will require a rethink of the current two-tier system of medical care offered by the University of Louisville. It appears the safety-net community as a whole is taking steps to make itself more attractive and responsive to the public it serves. That is something I have advocated for and I give them credit for any efforts.
Who gets how much and for what?
The sharp observer will notice that the state gives more money per beneficiary to different MCOs, and even to the same MCO in the separate payment areas. For example, In Region 3, Passport receives $458.43 per member/per month, the highest overall rate for an MCO anywhere in the state! Additional variation exists even for the same company! For example, Coventry gets $422.74 for its patients in Region 3, but only $395.80 for members in the rest of Kentucky. WellCare has the situation reversed. It gets a higher $438.38 out in the state, but only $381.30 in Region 3. What is going on? These companies all submitted bids for their services as part of their application to the state. Are some companies harder negotiators than others? While that may be true, it cannot completely explain these differences, based as they are on 27 different categories of patients in 8 different regions and not just on their raw numbers. Some categories of patients are predictably more costly to take care of. For example, disabled and elderly patients are more costly to serve than well-mothers and children. The aggregate rate shown in the table appears to be a division of total payment divided by the aggregate uncategorized number of beneficiaries. Both the relative lack of transparency as well as the raw complexity of the process makes it virtually impossible for a mere human like me to take it all in. I am not convinced that even the “experts” have as good a handle as they need. Whether the MCOs were accurately informed about the makeup and historical costs of the panels of patients they bid on and accepted has led to bitter disputes between the MCOs and the Commonwealth which have been held before the public eye and courts. I do not know if that is a problem that can truly be fixed across a broad geographic area.
You can’t make a proper diagnosis without a full history and examination.
The pubic who ultimately finances this system with our state and federal taxes has a right to better understanding. For example, why does Passport and its chief sponsor UofL get paid more than any other broad category of MCO? Are their patients sicker, or are they still receiving the supplementary payments from the state that they have enjoyed for so long under the rubrics of education, research, special services, consultation, etc. Are clinical monies still being used for non-clinical activities? Are our Louisville neighbors really in that much worse shape than our cousins in Appalachia? (That would be a surprise to me.) Who can point me to an authoritative accounting of who is paying for what and how much? If not, why not? Did Kentucky Spirit really get paid less than they deserved? If we cannot understand this as a public, how can we tell if Medicaid managed care is saving us any of our scarce resources, let alone taking good care of our neighbors?
Lack of transparency and accountability has been destructive to the reputation of our local University and its School of Medicine and which have stained Passport with their shadow. There have been too many below-the-radar deals made involving Kentucky Medicaid over the years. The current commotion over the pseudo-decrease in the public QCCT public funds that pay for some inpatient care at University Hospital is a good example of what can happen when all the facts are not on the public table. The Federal Medicare program is castigated by many for a variety of both valid and invalid reasons, but it has been a leader in transparency and accountability. Its numbers are out there for all to see. Our state Medicaid programs need to follow the lead of Medicare in this regard.
Peter Hasselbacher, MD
President, KHPI
Emeritus Professor of Medicine, UofL
June 26, 2013