Long live the Prince.
He gave us the gift of his music. Might he give us anything else? Is there anything to be learned from his untimely death? As of this writing, there’s no longer any doubt that he died of opioid narcotic poisoning – more specifically of fentanyl overdose. It has also been reported that his addiction to opioids was long-standing, even as it was well hidden from his public. Current popular accounts attribute his opioid addiction to prescription drugs that were begun to treat unspecified injuries related to his vigorous stage performances– as if this somehow automatically legitimizes the use of opioids for musculoskeletal injury or chronic degenerative disease. A claim that “I can’t live without my opioids,” is in my experience generally a symptom of the opioid dependance itself, not the underlying disorder for which the drug was begun. That is why we use the term addiction. Of course there is a place in medical care for narcotic opioids, but we have strayed far from that place today.
Fentanyl is the new bad boy.
Many other current reported deaths attributed to opioid overdose involve fentanyl, either by itself, or added to preparations of heroin. There has been no evidence reported that Prince was a heroin-user, although the investigation into the circumstances of his death is not over. Fentanyl is, milligram per milligram, the most powerful opioid available on the market. It is well known that its potency takes some opioid users by surprise with not-infrequent fatal results. (A weekend full of deaths in a given community is commonly the result of a fentanyl-augmented batch of heroin.) It is not yet publicly known how long Prince might have been taking fentanyl. Did he come by his fentanyl illegally? Was it provided to him unlawfully by friends or supporters who obtained the drug in otherwise legal ways? Was the unscheduled landing of Prince’s airplane the day he died the result of a fentanyl surprise, or had he not yet been exposed to the drug. Did he acquire the medical disadvantage of being a “special” patient? I suspect we will find out. I also suspect that he acquired his fentanyl the same way innumerable other patients do – from their own local healthcare providers. Often, but certainly not always, the initial exposure to opioids is done with the best of intentions. In Minnesota, there are a few providers who have written colossal numbers of fentanyl prescriptions. From publicly available data, it does not appear that the physician whose name has most often been associated with Prince’s death is one of those.
What physicians have been associated with Prince’s final days?
It may well be that the widely-traveled Prince has been served by many other healthcare providers over the years of his career. In recent accounts of the events leading up to his death, the names of two physicians have been prominently mentioned. The first, who attended to Prince at least shortly before his death, but may not have personally seen him that day, is a Minnesota family practice physician named Michael Schulenberg. I am unaware that Dr. Schulenberg ever provided opioids for Prince, but he appears to be under scrutiny by Minnesota authorities and has essentially fallen off the radar screen. The second is Dr. Howard Kornfeld, a pain and addiction management physician in Mill Valley, California. It is reported that he prescribed or was attempting to dispense Suboxone to Prince as a treatment for opioid addiction. No doubt, the full facts will emerge, and who knows, may even become public.
Suboxone and DAT.
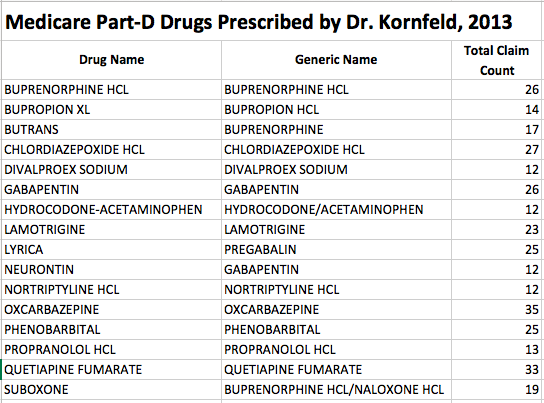
Suboxone, like methadone, is a drug increasingly being used to treat opioid addiction as part of drug assisted treatment (DAT). The total cost of DAT is rapidly becoming a major problem for state Medicaid and other insurers. Ironically, Suboxone and its basic ingredient, buprenorphine, are currently more heavily regulated then is fentanyl or any of the other commonly used or overused opioid! Only a limited number of prescribers are licensed to prescribe Suboxone, and then only up to as many as 30 or 100 patients. It is easier to hand out OxyContin – Go figure! Dr. Kornfeld is, as of this writing authorized to prescribe Suboxone or buprenorphine to patients for DAT. Dr. Schulenberg is not.
Why am I writing this?
When I read about unusual or outlier medical events in the media, my habit in recent months has been to look at the various payment and utilization databases made available by the Center for Medicare and Medicaid Services(CMS). These provide details for the public at the level of the name of individual providers and are unique in this regard. They tally the number of medical services or drugs provided or prescribed more than 10 times by a single healthcare professional for fee-for-service Medicare patients or Part-D Medicare drug benefit insurance programs respectively. These beneficiaries include both the elderly over 65, and the disabled of all ages. I have demonstrated that practice patterns of opioid prescribing to these Medicare patients are generally predictive of how drugs are prescribed to other patient populations. I have recommended paying attention to outliers both as a strategy to improve public health and to identify waste or abuse. Looking at outliers is fundamentally nonjudgmental because it can highlight efficiency or exemplary quality of care. On the other hand, looking at far-outliers also brings to light inappropriate medical practice or fraud. In my experience so far, extreme outliers either suggest or confirm trouble.
What can we learn about opioid drug utilization in Minnesota?
As occurs nationally and in individual states that I have examined in detail, opioids as a group are among the very most commonly prescribed drugs. A given single opioid preparation may be the most frequently prescribed drug for an insurance program. Although opioids are often thought associated with pain management or cancer doctors, the vast bulk of opioids are prescribed by generalists: Family Physicians, General Internists, Nurse Practitioners, and Physician Assistants.
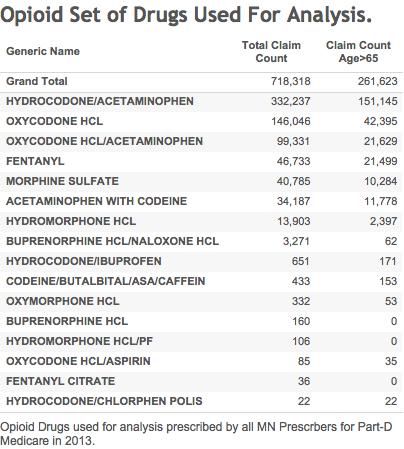
Medicare considers 2727 of 15,714 MN prescribers to be Family Practitioners in the Part-D prescription drug dataset. Of these, 2040 prescribed at least one opioid more than 10 times to one or more unique beneficiaries. For this analysis, an opioid was defined as a drug in which the generic name of the active agent contains the string ‘cod’ or ‘morph.’ I have previously described that this search picks up all the usual suspects. Fentanyl, Suboxone, and buprenorphine were also included. The list of all opioids I was able to identify that were prescribed by Family Practices is listed here.
All of the figures and tables referred to below are available for interactive viewing at my pages on Tableau Public. Selected links and static versions will be placed below as well. The first is an interactive Treemap datavisualization of the aggregate number of prescriptions for all Part-D drugs prescribed by all Minnesota prescribers in 2013 (the most recent year for which data is available.). The size of the data cell depicts the number of prescriptions, and the shading the total cost. The 16 different opioid preparations prescribed are grouped together as one entry and fill the largest cell. Fentanyl is the 4th most commonly prescribed opioid. (Check out the total cost of a single brand of insulin!) A similar Treemap for Family Practice has the opioid group squeezed down into a close 5th place by individual drugs used to treat cholesterol, blood pressure, thyroid, and stomach acid. The Treemap for Dr. Shulenberg is comparable  to that of his Family Practice colleagues. As might be predicted and is typical for medical practitioners, he has chosen a different set of drugs to treat common disorders. His prescribing of opioids appears swelled by hydrocodone/acetaminophen, but the absolute numbers are small, subject to statistical variation, and will be discussed in further detail below.
to that of his Family Practice colleagues. As might be predicted and is typical for medical practitioners, he has chosen a different set of drugs to treat common disorders. His prescribing of opioids appears swelled by hydrocodone/acetaminophen, but the absolute numbers are small, subject to statistical variation, and will be discussed in further detail below.
What kind of practice?
In terms of outpatient drugs for which more than 10 prescriptions were written, Dr. Schulenberg’s 2013 Part-D outpatient medication list appears to me to represent a profile of a typical Family Physician. His payments from Medicare for general medical services in 2013 (CMS data limited to Fee-For-Service Medicare patients only and exclude managed care) are solely for brief- and limited office, and nursing home patients. The number of unique beneficiaries served cannot be calculated but would appear to fewer than 100 and certainly less than 200.
His drug utilization list drug list suggests patients with the common disorders seen in general practice. On the other hand, Dr. Schulenberg did prescribe significant numbers of prescriptions for opioids, especially the combination drug hydrocodone/acetaminophen (a.k.a. Vicodin or Lortab) which was the most commonly prescribed opioid prescribed in MN for all specialties combined. (See table.) However, based on available CMS data alone, it cannot be said that he is a far-outlier in this regard. With respect to fentanyl, the fourth most prescribed opioid in Minnesota in 2013, Dr. Schulenberg prescribed far below the average raw number of prescriptions compared to other Family Practitioners using fentanyl. A major caveat to these conclusions is that rates of prescribing cannot be calculated because of patient confidentiality protections built into the database. Counts of patients are not provided when their numbers are less than 11 for a given service or drug.
Opioid utilization compared in detail.
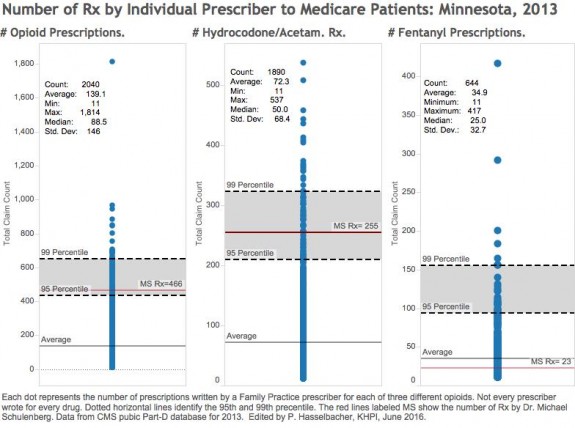
In 2013, Dr. Schulenberg wrote 466 prescriptions for 6 different opioids comprising 7.9% of all drugs prescribed by him more than 10 times. For all identified Minnesota Family Practice opioid-prescribers, these figures were 283,730 prescriptions for 16 different opioids comprising 4.2% of all prescriptions (3.9% if non-opioid prescribing Family Practitioners are included in the calculation). The average number of total opioid prescriptions per prescriber in the Family Practice group was 139.1 with a standard deviation of 146.0 The range was 11 to 1814 prescriptions. The median number of prescriptions was 88.5. Note that the distribution of the number of opioid prescriptions by prescribers is not statistically “normal.” A minority of prescribers write for the large majority of opioids. However, whether by percentile rank or standard deviation, Dr. Schulenberg is not strictly-speaking, a statistical outlier. Many other Family Practice professionals prescribed more opioids than he did. It is interesting to note that if two off-the-chart pain management providers with total opioid claim counts of 1,611 and 1,994 are excluded, the average and mean number of prescriptions are hardly different from those of Family Practice!
Statistical Comparisons.
Here is how Dr. Schulenberg compares to other Family Practice prescribers for all opioids combined, for hydrocodone-acetaminophen, and for fentanyl. For the first two items his raw numbers of prescriptions lie somewhat above 95th but below the 99th percentile of all Family Practice prescribers. For fentanyl, his raw number of prescriptions is well below average.
What is happening at the top?
If I were looking for extreme outliers in the Family Practice group, I would be looking at other prescribers first. At the top of list is a prescriber who wrote a jaw-dropping 1814 prescriptions for opioids– 10.5 standard deviations above the average for all family physicians. Another wrote 417 prescriptions for fentanyl. I notice also that several nurse practitioners and physician assistants were also very heavy prescribers of opioids. Do these prescribers work in a hospice facility? Are they part of a pill mill? The Medicare Part-D database identifies every prescriber by name– anyone can know. A quick look by the Minnesota licensure boards could tell the tale. There are certainly legitimate reasons to prescribe opioids, including to dying patients. However, there is no dispute that there are some grossly inappropriate or frankly illegal opioid-prescribers out there. It is my opinion that if the terrible national problem we have with opioid addiction and abuse is to be solved, we need to grapple at the prescriber level where the first doses of opioids are being given by generalists. Focussing on pain management doctors or pill-mills is negligently insufficient. Should I have published a list of the actual names of the prescribers here? Give me your advice.
What about Dr. Kornfeld in California?
There are no entries for him in the 2013 Medicare Payments to Providers database. If he was in practice in 2013, he may not have billed any Medicare patients. He did however write prescriptions to beneficiaries who were enrolled in Medicare Part-D insurance plans. He wrote prescriptions for 16 individual drugs to more than 10 patients each (See table) but not more than 33 prescriptions for a single drug. The drugs prescribed seem typical of a pain management/addiction practice and were not limited to opioids. Buprenorphine was on his list, but fentanyl was not. No doubt regulatory or law enforcement authorities are looking into his involvement in the death of Prince, including whether or not his practice lies within the wide boundaries of accepted medical care. I have no basis upon which to offer an opinion and do not do so.
Other Observations.
Old or disabled?
For Minnesota as a whole, the majority of all opioids are prescribed for disabled beneficiaries, not for the elderly (or not-so-elderly-feeling) beneficiaries over 65 years old who we usually think of when we think about Medicare. I suppose this is not surprising. Disability and addiction feed upon each other. Aside from addiction potential, it should be well known that opioids are not as safe for use in the elderly. Conversely, only a tiny proportion of buprenorphine was prescribed to the elderly. Curiously, fentanyl was the individual opioid given to the highest proportion (46%) of elderly. Perhaps this is indicative of the prevalence of cancer in this population.
Where are Opioids Prescribed.
Shown here is a list of Minnesota cities in which opioids were prescribed ranked by the number of prescriptions. It is no surprise that it is cities where there are lots of people and healthcare providers that the most opioids would be prescribed. However, when the rate of prescriptions per unique opioid prescriber in a given city is calculated, a very different result is seen. Small places with one or a few prescribers head the list in terms of rates of prescriptions. I left the on-line list long for this reason. What is this data trying to tell us? Are small town providers facing impossible-to-resist demands? Is a different standard of care being provided in these places for whatever reason? I am not familiar with the demography of Minnesota. In Kentucky, Indiana, and Ohio, several very small places stood out like a sore toe because of their volume of opioid prescriptions. It looks to me like that is the case in Minnesota as well. To my inspection, some of the top opioid prescribers worked in such places. Perhaps a Minnesota “local” will point out some discrepancies or explanations for us.
What specialties prescribe the most?
For completeness, and for the interest of Minnesotans, I include a full list of the number of opioid prescriptions by the specialty identified by Medicare. Below is a list of the Top 20 by total claims (Rx).
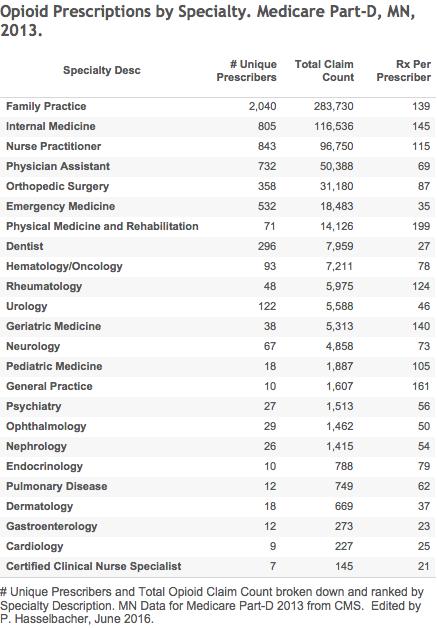 These data allow a calculation of the average number of prescriptions per unique prescriber in that specialty. Note that in specialties with few members, that a single prescriber with large numbers will markedly skew the average upwards. Thus for Interventional Pain Management, if a single prescriber is omitted from the calculation, the average falls from 205 to 138. In the Pain Management specialty with the highest prescriber omitted, the average drops from 495 to 121. Without the two high-rollers, the averages from these pain-intensive specialties fall below the rates for the major general medical practices What is that telling us!
These data allow a calculation of the average number of prescriptions per unique prescriber in that specialty. Note that in specialties with few members, that a single prescriber with large numbers will markedly skew the average upwards. Thus for Interventional Pain Management, if a single prescriber is omitted from the calculation, the average falls from 205 to 138. In the Pain Management specialty with the highest prescriber omitted, the average drops from 495 to 121. Without the two high-rollers, the averages from these pain-intensive specialties fall below the rates for the major general medical practices What is that telling us!
I was surprised to see the average rate for Hospice and Med-Onc to be so much lower than for generalists. It is these former specialties that we are inclined to allow the most discretion for the use of opioids. Most surgery specialties are low. I was surprised to see Pediatric Medicine up there, and was personally both surprised and disappointed to see Rheumatologists at the upper end of the list. In my many years in academic rheumatology, I cannot recall any credible authority advocating the use of opioids in our day-to-day work. In fact, the recommendations were against the use of opioids and I would be surprised to find that philosophy to have changed. I don’t know what to make of Anesthesiology. Many in this specialty are heavily involved in pain management. Indeed, the other pain management specialties took their lead from anesthesiology. We must also assume that some of the Family Practice prescribers in the data are functioning as pain management practitioners. Why would Manipulative Osteopathy be third on the list? I thought this specialty did not depend on drugs. In short, looking at data such as these often raises more questions than answers– which is exactly the reason we should be looking!
In conclusion.
What we did not learn in this exercise is who might have given Prince the fentanyl that took his life. Nor do we know where he obtained the opioids that led him into a life of opioid dependance. The truth is, that we would not have had a chance to learn such things from this database in any event. It appears to me that the physician who was reported to have at least attempted to attend to Prince near the time of his death was not even an average prescriber of fentanyl– at least not to disabled or elderly Medicare patients. While I suspect answers will be found, patient privacy or other medical and legal considerations may limit what the public ultimately learns.
I predict that Prince will be found to have been a casualty of our every-day medical system with respect to how opioids are used. Examination of the Minnesota data confirm what I have written about in other states. That for a variety of reasons, opioids are at or near the top of the list of the most frequently prescribed drugs. Our nation is flooded with opioids. I show again that the bulk of opioids enter our communities not through pain doctors or pill-mills, but through the offices of general medical practices whether they be staffed by physicians, nurses, or physician assistants. I present again the striking variation of opioid prescribing within a given specialty– a variation that I cannot conceive is justifiable by medical necessity. The variation among providers is trumped by geographical variation such that some small cities hand out more opioids than much larger ones. What is going on there? Is anyone looking? Has all of this been going on unnoticed? Absolutely not!
The argument by our professional lobbying organizations that our prescribing histories are private won the day for too long. We were given unwarranted deference despite demonstrable evidence that self-governance was not adequately successful. For example, in Kentucky our KASPER system of monitoring the dispensing of opioids and other controlled substances was set up to ultimately fail in this regard. It was targeted to patients and opioid users rather than professionals. Law enforcement, state administrative, and licensing organizations were and still are specifically prohibited from looking for outlying professionals. KASPER did work to shut down some pill-mills and doctor-shoppers, but it did not address the root of the problem– that too many health professionals prescribe too many opioids to too many patients, and that our professions and professionals have not effectively moved to intervene when we see a problem. To my understanding, current legislative and administrative efforts to deal with the national epidemic of drug abuse and deaths emphasize treatment and education. That is necessary, but I do not believe this will have much effect until we as a society grapple with ways to reduce the number of initial opioid exposures. This means getting down in the trenches. This will in my opinion mean looking at outliers, verifying that acceptable medical practice is occurring, and if not, intervening in an effective way that may require more than education. It cannot be said that we do not know where to look. I reject categorically the argument that more supervision and accountability will deny justifiable opioid treatment to patients who have a chance to benefit. No responsible healthcare professional or organization would allow that to happen.
A recent mass murder of historic proportions in Orlando has not apparently generated enough public demand to do any thing differently than we do now. Opioids are killing a lot more people in America today than guns. It may well prove to be impossible to identify smoking-gun involvement by any individual medical provider in the fatal opioid overdose of Prince In my opinion, the current national standard of medical care itself is fueling our drug abuse catastrophe. If we fail to demand more transparency and accountability from the professionals we entrust to provide these drugs to patients who actually can benefit from them, I reluctantly predict that opioid addiction and deaths will continue to increase. We might as well just decriminalize opioid use and allow it to be purchased and used safely as we do for alcohol and tobacco which individually kill even more of us. At least the disease and crime that are the camp-followers of opioid abuse would not exponentially amplify the collective human misery caused by the drugs themselves as now occurs. What happened to Prince has happened to other outstanding musicians and artists before him and is happening to uncountable thousands of the rest of us today. We should not have needed his death to remind us how bad things are.
Peter Hasselbacher, MD
President, KHPI
Emeritus Professor of Medicine, UofL
27 June 2016
Bear with me and let me know if any links are not working right. Tableau is still new for me. As a test, I have embedded all the interactive data visualizations just below. Let me know if this causes a problem with portable devices or download speeds, or if I should leave the interactive versions off site.

One thought on “How Did Prince Get His Opioids?”
Comments are closed.