A society is only as healthy as the sickest individual within it.
Summary:
Kentucky is in the middle of, and hopefully emerging from a major epidemic of Viral Hepatitis-A (Hep-A). Hepatitis-B and Hepatitis-C, are caused by different viruses and commonly result in more serious chronic liver disease. Classically, the spread of Hep-A is attributed to contamination and ingestion of food or water by the feces of infected persons or related poor hygiene practices. Nonetheless, illicit drug use appears to be the major risk factor in Kentucky’s current outbreak. Hep-A is rarely fatal to otherwise healthy people but can cause debilitating symptoms. It can be fatal however, especially to individuals with preexisting liver disease such as alcoholic hepatitis or other forms of viral hepatitis. It is not clear when the first cases of the current outbreak began to emerge, but in the 21 months between Aug 1, 2017 and Feb 23, 2019; some 4229 presumed or suspected cases of Hep-A have been reported, including 2036 hospitalizations and 43 deaths. This can be compared to only 9 reported cases in all of 2016! Our current outbreak is the most severe in the nation. Concern has been expressed that, compared to the aggressive and successful response by the Board of Health of Jefferson County, that the best advice from experienced state public health experts within Kentucky’s Public Health Department in Frankfort was ignored allowing the statewide epidemic to expand and be prolonged. My independent analysis of available data supports this criticism. In my opinion, the appointment of an inexperienced public health commissioner by the Bevin administration– probably for political and ideological reasons– likely played a significant role in what occurred. Kentucky remains in the middle of upsurges of Hepatitis B and C. All three varieties of viral hepatitis have roots in poverty, substance abuse, exclusion from healthcare systems, despair, and other non-medical fellow-travelers that will be difficult to fix. It is therefore important that the current responses to the Hepatitis-A epidemic be independently reviewed so that we may be better prepared for the next time– which will surely come.
I am a believer that real-time monitoring of healthcare events and outcomes serves a useful public function whether it be it how or where opioid narcotics are prescribed, or in the reporting of communicable diseases. The promise of such surveillance implies that broad-based systems exist to collect reliable information in a timely way and that there exists sufficient societal willingness and the means to do something with the information. Sadly, our healthcare non-system is insufficiently equipped or empowered to adequately fulfill either of these latter requirements. We seem often too late to identify a problem and too late to respond– if at all.
Viral disease outbreaks in Austin were no surprise.
For example, small-area mapping technology using Medicare public-use files disclosed that the town of Austin, IN was a hot spot for the excessive prescription of opioids several years before that small city became the nation’s poster-child for epidemics of HIV and hepatitis infections, and for opioid addiction. In 2016 I wrote about the explosion of reported cases of Hepatitis C and Hepatitis-B in Kentucky that began around 2010, leading the nation in this regard. Kentucky was already in the unenviable a position as a leader in the promiscuous over-prescription of opioids that amplified these disease epidemics. It has long been recognized that substance abuse, hepatitis, and HIV infection are fellow travelers. In these circumstances, there is no excuse for not giving more attention to the incidence of new cases of hepatitis of any viral cause the highest statewide priority. I wish I was more confident that our disjointed and under-funded public health system was up to the task. The current series of investigative reports by Laura Unger, Chris Kenning, and others in Louisville’s Courier-Journal allow a reasonable person to conclude that Kentucky’s public health system let us down, and that calls for review by legislators and other public officials to explore what has happened and why are justifiable.
Control of public health information implies special responsibility.
Acute viral hepatitis is a reportable disease. That means that healthcare entities have a legal responsibility to report new cases to some public health organization which is supposed to keep track of such things. We fail badly in this regard. The Center for Disease Control and Prevention (CDC) is the federal agency responsible for collecting what the individual states submit and to analyze that information scientifically. Sadly, CDC funding and its mission is being strangled by anti-science and small-government forces. Even in the best circumstances the CDC must work with dated and incomplete information. Individual states face the same problem. It is estimated that the true incidence of viral hepatitis is as much as 20-times higher than reported existing disease-counts. A few reportable cases are likely only to represent the tip of the iceberg. Prompt identification of isolated outbreaks of infectious diseases therefore remains critically important but handicapped.
Hepatitis in Kentucky: 2000-2016.
In preparation for this article I wanted to update the graphs and maps I made in 2016 from CDC counts of Kentucky’s reported cases of Hepatitis-B and C, and to include Hepatitis-A. The CDC data available to me in 2016 was only as current as 2013. There is still a lag of more than two years! More current data for the Hep-A epidemic is now available on the website of the Kentucky Public Health Department. Once you start looking for something, you will find more of than you expected! [Click on the figures to enlage them. Interactive versions will be posted elsewhere when i get a chance.]
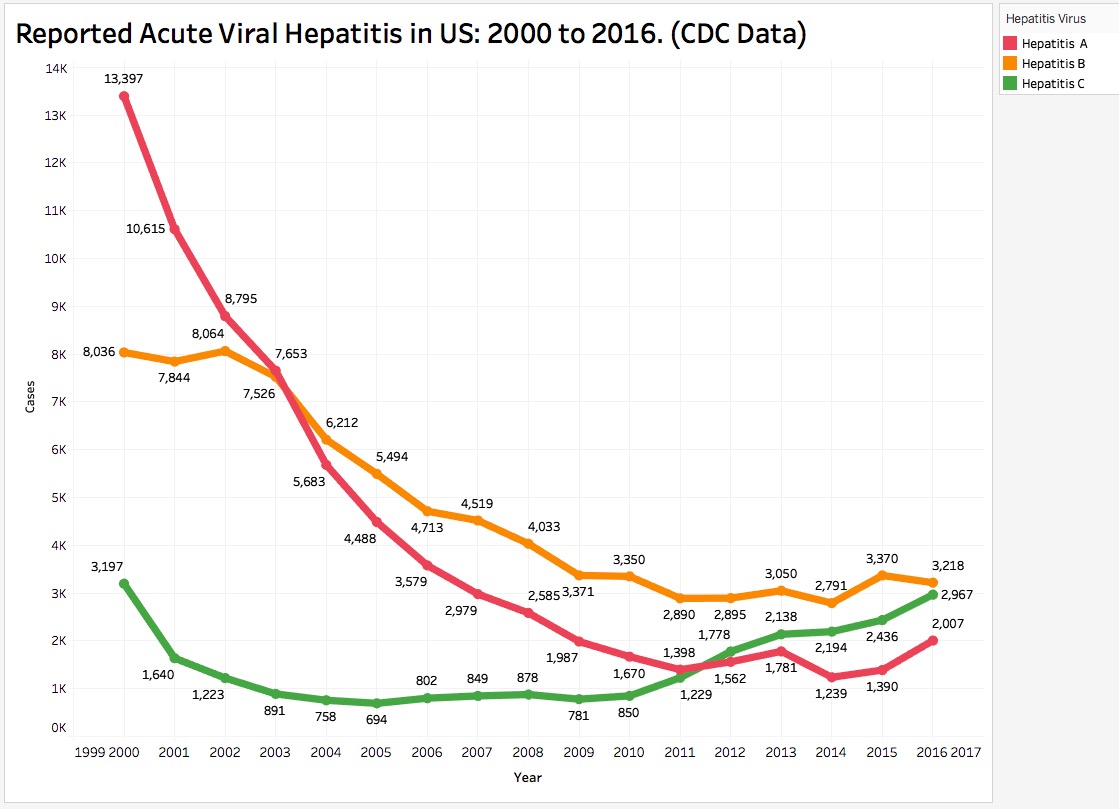
The most recent CDC data available to me was current only to 2016 but was collected in the same way and is therefore comparable to previous years. The national data show major decreases in the number of reported cases of all three major viral forms of hepatitis from 2000 to around 2009. In 2009 reported cases of Hep-A and Hep-B appear begin to plateau. Reported cases of Hep-C on the other hand, begin to increase, perhaps related to intravenous substance-abuse. Vaccines for Hep A and Hep-B have been available– but not for Hep-C. One would like to believe that made a difference!
Extracting the numbers of reported cases in Kentucky from the CDC data reveals a much different picture. Beginning around 2007, reported cases of Hep-B and Hep-C began to spike. Both of these are commonly acquired through exposure to contaminated blood, as by needles. The incidence of neither of the two viral causes of hepatitis has fallen to their historically recent lows, and the incidence of Hep-B may even be increasing further. We are still in the middle of those outbreaks and their full individual, social, and financial burdens have yet to be borne. (In addition to the personal burdens of individuals, thins about the colossal cost of anti-viral hepatitis drugs, liver transplantations, and hospitalizations.) Curiously from the perspective of this article, following an outbreak of cases in 2001, the reported incidence of Hep-A (not really a blood -borne disease) has continued to trend downwards with only 9 cases reported in all of 2016. Of course, these observations hinge on the validity of the data. What does not get looked for and reported does not get found!
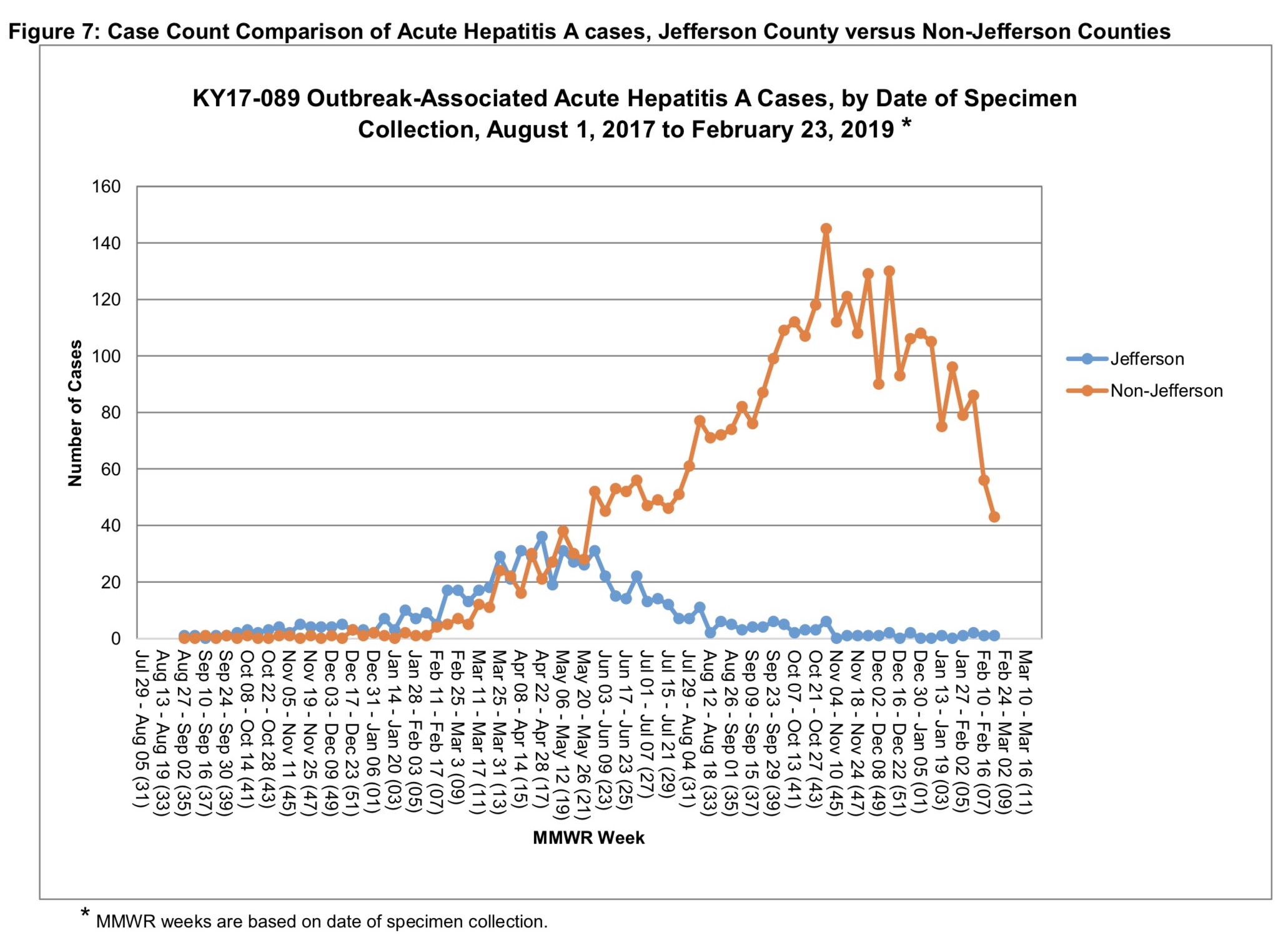
I looked on the website of the Infectious Disease Branch of Kentucky’s Department for Public Health– Division of Epidemiology and Health Planning for more current numbers specific for our Commonhealth. Many of the links were broken, but the Infectious Disease Branch has been posting weekly reports of reported cases with charts and maps currently summarizing cases between Aug 1, 2017 and Feb 23, 2019. Between these two dates the Division reports a total of 3063 confirmed and probable cases of Hep-A with an additional 1166 suspected cases for a total of 4229 cases. Of these, 2036 were hospitalized with 43 deaths so far. [A figure from the most recent report is shown below.]
The highest weekly statewide tally of about 150 occurred in early November 2018 but by February 2019 were as low as 40 per week statewide. The weekly tally of cases from Jefferson County peaked at about 40 in early May 2018 and rapidly declined to few or no new cases since August 2018. Recall that in 2016 the CDC data showed only 9 reported cases of Hep-A for the entire year. By the fall of 2017, case-counts from Frankfort were already exceeding that number weekly! One might argue that an increase in cases in the state as a whole might have been noticed earlier, but that would require we have an integrated public health system providing continuous scrutiny rather than a “partnership” of semi-independent local public health agencies within which which the bigger picture is vulnerable to be missed. We are all in this together folks!
The Frankfort graphs are compatible with assertions that aggressive responses to the outbreak in Jefferson County allowed it to turn the corner, while something less than an appropriate statewide response allowed the Hep-A epidemic to blossom. Hopefully we have turned the corner in Kentucky, but the underlying public health and societal problems remain, and we are vulnerable to additional outbreaks.
Let us not demonize the sick or poor.
I do not minimize the fact that there exists a huge number of non-medical determinants impacting who gets hepatitis and where. There should be absolutely no mystery or surprise that folks on the fringes of society most likely to contract viral hepatitis. It is no coincidence that such individuals are more likely to be excluded from our healthcare system and therefor our public health surveillance systems. Nonetheless, these people live among us and we are all vulnerable to these transmissible infectious diseases. A society is no more healthy than the sickest citizen within it. Understandably, no one is happy to take the blame for any putative failure to detect or respond to this serious outbreak/epidemic. Nonetheless, no offered excuses or justifications for actions taken or not taken should prevent a careful retrospective and independent review of the safeguards we have in place– or should have in place for the future. This epidemic is not the last one that we will see!
Who was running the show in Frankfort?
Much of the finger pointing so far has been directed at Dr. Jeff Howard, who in November, 2017 became Acting Commissioner and in July 2018 was appointed to Commissioner of the Kentucky Department of Public Health. All of this fell into his lap. His academic background is impressive. He graduated from Union College of Kentucky, and in 2012 from the University of Louisville School of Medicine. According the Kentucky Board of Medical Licensure, Dr. Howard received a Kentucky medical license as a surgical trainee in June of 2018. He appears to have taken time out from medical training to enroll in a master’s degree in business administration at the Harvard T.H. Chan School of Public Health, said to be awarded later this Spring. Despite his obvious academic credentials and apparent enthusiasm; his appointment without previous independent medical practice experience, precious-little public health experience, and only a brief stand of acting administrative experience; he was setup for criticism by Governor Bevin or his administration. Some of this might have been tempered if Dr. Howard was surrounded and protected by more senior and experienced co-workers, but it seems clear that he ignored their strong advice about how to handle a serious emerging epidemic, or alternatively, did not have the clout to push back on the Governor’s Executive Offices. On the other hand, and less sympathetically, Dr. Howard simply followed orders from above.
No place for dogma.
It is one of my core beliefs, and that of contemporary medicine, that medical practice and public health medicine should follow proven science. Things that have been proven to work should be used. Things that have been shown not to work should be ignored. Things that have not been proven to work should be used, if at all, with caution. In this philosophy, there is no room for purely political, ideological, or religious intrusions into the practice of medicine– including public health. In my opinion we are seeing such intrusions, including as least some appointments by Governor Bevin of individuals with limited experience or extremist views to positions with medical oversight and control responsibilities such as the Board of Medical Licensure, the Board of Trustees of UofL, or perhaps even the Department of Public Health. The Governor’s or his proxies’ heavy-handed intervention in women’s healthcare operations at University Hospital has been no secret. In my opinion, experience and tolerance are being displaced as requirements for office to make room for the soldiers of Governor Bevin’s culture wars.
Of course, it is any Governor’s privilege to appoint people to government positions, commotions, or boards who are in agreement with his or her political philosophy. All Governors will ultimately be judged on the wisdom and appropriateness of their appointments. However, from his first day in office, Governor Bevin made it clear that he wanted to diminish if not remove the separation of church and state. In my opinion, he is doing just that. We are all free to have our own personal religious beliefs– or none. However, for all of recorded history to the present, it has been the goal of at least some religions to control government as a way to impose their ideology on other people. My back-of the-envelope calculations inform me that over the centuries, religion-fueled wars have killed– and are still killing– more people than all the plagues combined. The intrusion of religious or any other intrinsically non-scientific ideology into the practice of contemporary medicine and public health must be confronted and eliminated. I do not believe that is happening now.
Peter Hasselbacher, MD
Emeritus Professor of Medicine, UofL
President, KHPI
6 March 2019
As always, if I have made an error of fact, please bring that to my attention. The opinions expressed above are my own but all are free to adopt them!